BILLINGS — At its height, St. John’s United in Billings had 186 licensed beds as one of the largest nursing homes in the state. Today, that number is closer to 120.
You can find 16 of those 60 lost beds in one of their West End campus' transitional care cottages, once a haven for Montana's golden generation, now shuttered.
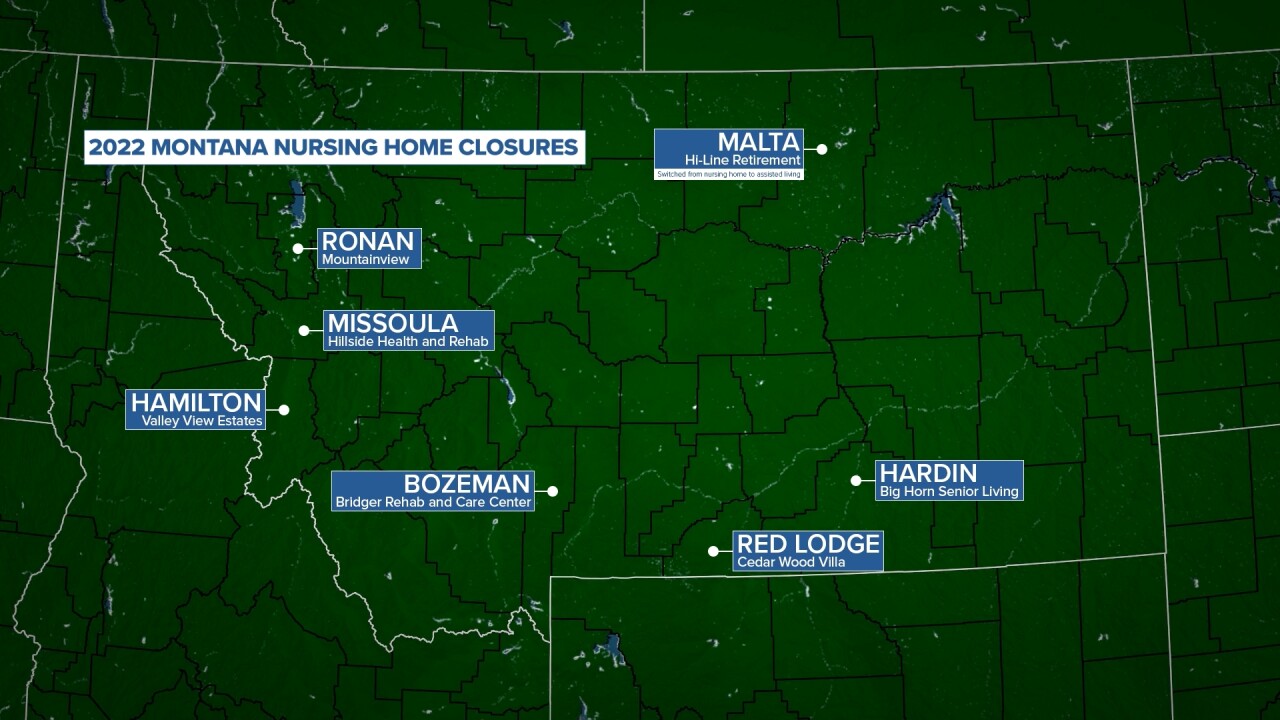
Seven other entire Treasure State nursing homes have been forced to close in 2022: three in western Montana, and one each in Bozeman, Malta, Red Lodge, and Hardin (Hi-Line Retirement in Malta transitioned from a nursing home to an assisted living facility.) And reduced beds in almost every one of the state's remaining homes is the equivalent to closing another dozen.
The reason is twofold: One, there are not enough trained professionals to staff the buildings; and two, Medicaid reimbursement rates set by the state legislature are nowhere near high enough to keep these businesses afloat.
"We're living in a totally different time over the last six years," said David Trost, President and CEO of St. John's.
In reality, Trost started to notice changes much longer ago - around 1997, when the Federal Government repealed the Boren Amendment.
"There were laws in place to require states to reimburse nursing homes for their cost," Trost said. "Those laws were repealed, which allowed states to pay nursing homes whatever they were willing to accept."
Trost, who was a nursing home administrator at the time of the repeal, said St. John’s nursing home wing was losing about $500,000 a year back then, a number they could cover. But now?
"Today those numbers are over $3 million for St. John’s alone," he said.

So six years ago, St. John’s started to change their model, reducing their number of beds in hopes to better allocate their shrinking resources. The empty cottage was closed as a COVID management tool midway through 2020, but when the facility went to re-open, their was no staff - and no money to pay for that staff - to do it.
"We’re competing with the types of businesses we didn’t compete with before," said Rose Hughes, executive director of the Montana Healthcare Association. "If you can earn $15-20 in a restaurant, that might be an easier job physically, mentally, emotionally than taking care of nursing home residents."
A lot of employees are being poached by nursing agencies which charge facilities up to three times more.
"We're paying certified nursing assistants $40, $50 an hour," Trost said, "but we’re having to pay some travelers to travel to Montana to serve us $110 an hour," Trost said.
"Most businesses can raise prices to accommodate paying their workers more," Hughes added. "With nursing homes, it all comes back to the fact that 70% of people are on Medicaid."
Medicaid is the principal payment source for long-term care in America, especially for low-income and elderly individuals. State legislatures determine what rate they will pay a nursing home for daily care of each patient.
"For St. John’s in 2020, our cost report said our daily costs were $320 a day," Trost said. "Our reimbursement was around $208 a day. That’s where our deficit of $3 million comes from."
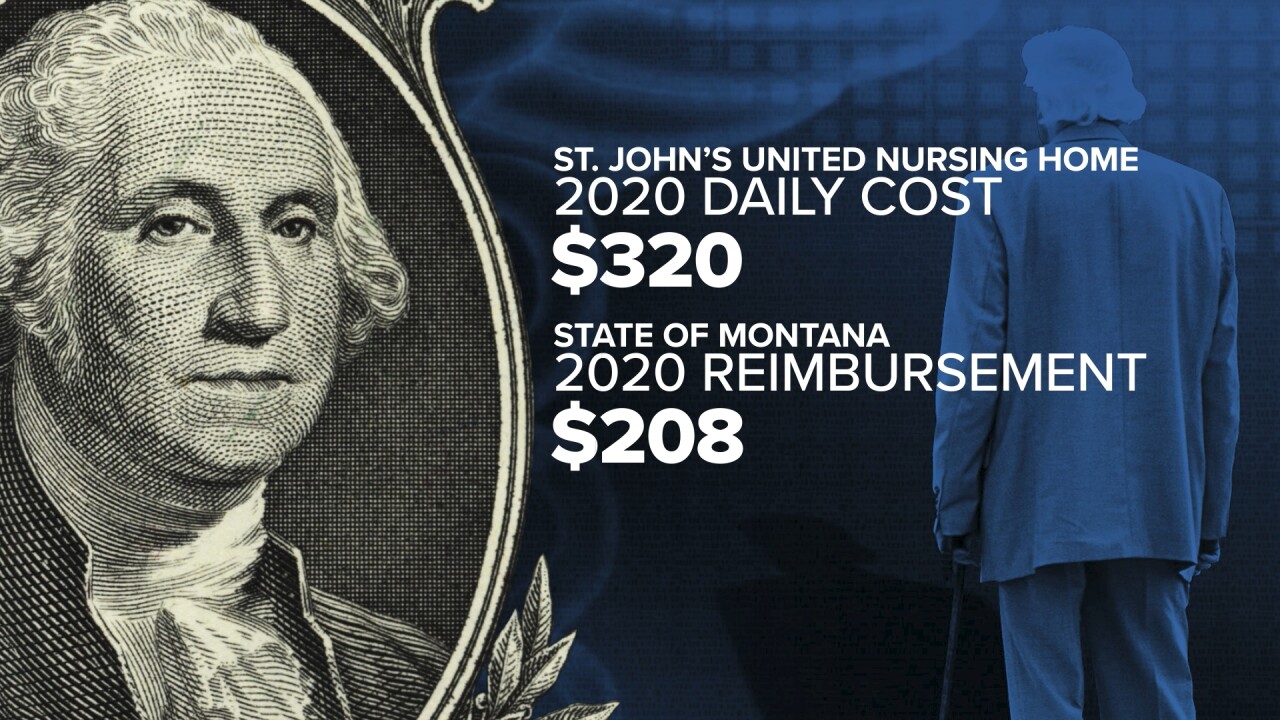
St. John’s latest rate for fiscal year 2023 - $214.13.
When asked why rates have not been raised to meet inflation costs, Montana’s Department of Health and Human Services said there were no current plans to add funding.
“The department has been clear about our intentions to address Medicaid provider rates, in collaboration with the Legislature," DPHHS told MTN in a statement. "The reality is the Legislature has not authorized additional supplemental funding for DPHHS to address rates at this time.”
Montana’s current administration says declining nursing home populations over the last decade show the current model isn’t working, especially in rural areas, and DPHHS has told providers to explore alternative models such as assisted living. But those facilities are only able to accept Medicaid patients through a waiver system, and most limit the amount they take.
"Why?" Hughes asked. "Because rates for assisted living aren’t what they need to be either. (DPHHS' study) shows those rates are 20% too low."

The state has a legal obligation to re-home Medicaid nursing residents of closed facilities, but as more and more close, those residents get farther and farther from the most important things in their life.
"When you separate them from their family, care will go down," Trost said. "Care is not just what we're able to medically provide our patients. It’s about our ability to connect with people who are a part of their support system. If they are moved away from them, (residents) will decline at a much faster rate."
Ultimately, providers say this disturbing trend will continue unless the state allocates significantly more funding to keep facilities open.
"This is only going to be solved if people agree that these people are worth caring for," Hughes said. "That's what it really comes down to - we have to decide if older people who are sick and don’t have the money are worth it."
"It's all in state’s control," Trost added. "It's whether they press the levers they need to press."




